Wednesday, October 8, 2025
The Independent Practice Advantage: Better Technology, Better Outcomes, Better Margins


Large healthcare organizations are trapped in a tangled web of red tape, which means they just can't keep up with how fast technology is moving.
This creates a major opportunity for independent healthcare practices to deliver better patient outcomes while improving their bottom line. While larger players face months-long (or even years-long) approval processes, smaller, independent healthcare practices can be more agile in adopting new administrative technologies that free up clinical time and reduce operational costs.
Christopher Gaskins, PhD, OTR/L, and CEO of mobile neurorehabilitation practice Neurosuite, knows what's possible when bureaucratic restraints are removed. The structure of his independent practice has enabled him to move quickly and implement solutions to streamline core processes, like scheduling and documentation. Now, he sees more patients per day while spending more quality time with each one—driving better outcomes for his patients and stronger revenue for his business.
But his PhD training in neuroscience and cognitive science has also shown him that speed must be met with careful strategic planning, especially when it comes to evaluating how technology impacts cognitive load and mental resources.
Key Takeaways:
- Large healthcare organizations face bureaucratic constraints that slow down tech adoption, leaving them with outdated solutions that waste clinical time and money.
- Independent healthcare practices can evaluate and deploy new administrative tools more quickly, translating to more patient visits and better quality interactions.
- But they need to make sure those tools align with how they work — otherwise, implementation will backfire, adding to the cognitive load on employees without improving care or profitability.
The bigger the practice, the slower they move—and the more they lose
For many hospitals and large healthcare organizations, the value of new administrative solutions is clear, and they're excited about the benefits these tools offer: increased efficiency, satisfied staff, and better patient outcomes.
But their internal structures make adoption difficult. Thanks to highly bureaucratic procedures, months or years can pass between identifying a problem and fully implementing a solution. And as time goes by, the solution they're evaluating gradually becomes more obsolete.
This lag in approval leaves healthcare organizations with outdated administrative tools, even for routine tasks. Gaskins notes that he still needs to send faxes to some hospitals, given that they won't accept encrypted emails.
The impact of slow-moving operations and outdated solutions extends beyond inefficiency or even staff frustration. They directly compromise patient care and drain practice resources. Gaskins recalls evaluating a patient's home and observing several safety risks, including a hole in the ceiling and widespread clutter. He documented the dangers and submitted the report to the case manager via the established system.
A year later, the case manager called to ask about the evaluation, meaning the patient never received the immediate follow-up attention they desperately needed—a care gap that could have been prevented with better administrative systems.
Better care, better margins
This sluggishness creates an opportunity that many independent practices don't fully recognize. While large organizations deliberate and run through countless review cycles with a wide variety of stakeholders, leaner, independent practices can evaluate and deploy new solutions quickly—and that speed translates directly into improved patient outcomes and stronger financial performance.
Referencing this agility, Gaskins says, "This is why I value having a small business, a small healthcare business. Because we can move. Obviously with proper compliance, we can move with speed and agility to implement the software we need."
When Gaskins finds a tool that can help him tackle administrative pain points, he can put it in place without having to jump through hoops to secure approvals. In fact, he's already developed and launched an innovative AI-driven solution to support appointment scheduling for his mobile practice—and the business impact has been substantial.
With his patient base spread across the DMV area, Gaskins initially had difficulty with travel logistics. Getting to each of his patients required a 15- to 40-minute commute, and he also had to take their time-of-day preferences into account. His AI-driven solution automatically groups his patients by location and suggests optimal scheduling times, factoring in any timing preferences.
The results speak to both care quality and business performance: he's reduced scheduling time and increased his daily patient capacity, which directly improves revenue per day. Just as importantly, eliminating this administrative burden allows him to reserve his mental energy for more personalized and in-depth patient interactions.
He can spend more time understanding each patient's specific needs and goals, leading to better treatment plans and outcomes—without sacrificing productivity.
However, while moving quickly is possible, independent practices still need to be thoughtful. They must take great care to select the right administrative technologies for their specific practice. Otherwise, Gaskins highlights that implementation will backfire, creating more work for employees while introducing compliance risks—ultimately hurting both patient care and the bottom line.
Pick solutions that work for you, not against you
When administrative solutions don’t align with existing workflows, they’re difficult and confusing for employees to use. Rather than boosting efficiency and freeing employees to take on higher-value tasks, their presence disrupts day-to-day work and adds to the cognitive load on employees by forcing them to develop complex workarounds just to get through the day.
Due to his neuroscience training, Gaskins understands the issue (and how to avoid it) better than most. “Even with technological advances, technology is not always being implemented correctly. This ends up placing more cognitive load on the user without the added benefit of improved performance,” says Gaskins, drawing from his research background.
That’s why independent practices should take the time to understand their existing processes before evaluating new solutions, with a focus on the workflows that take the most time or generate the most errors. Gaskins maps them out, often using visual diagrams, to understand how they operate and where bottlenecks exist. This helps him determine the types of solutions he needs and the specific features they must have.
Want to learn more about how Gaskins combats cognitive load at his neurorehabilitation practice? Take a look at this playbook.
For example, a close look at his own operations showed him that scheduling was proving particularly problematic, leading him to prioritize finding a solution to address it. And it couldn’t just be any scheduling solution either. It needed to be able to handle appointments for patients across an expansive geographic area with varied timing preferences.
Once he completes the process mapping exercise, Gaskins uses the checklist below to evaluate potential contenders. By checking off each box, independent practices can ensure that new solutions will blend smoothly into existing operations while meeting compliance standards.
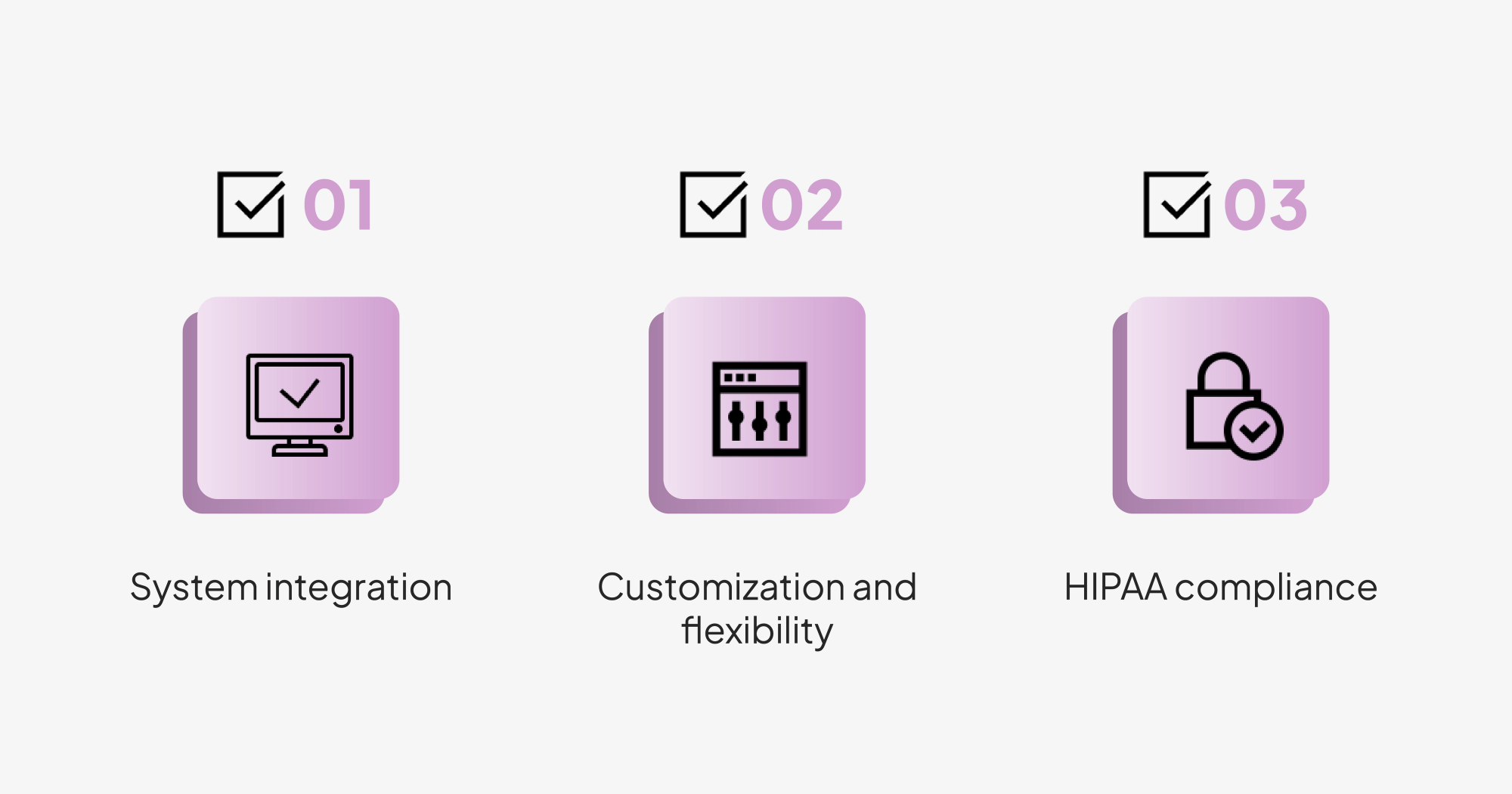
- System integration: New administrative solutions should be able to connect to and interact with existing software. This helps prevent bothersome workflow disruptions, like the need to duplicate data entry and constantly switch between systems.
- Customization and flexibility: Practices should look for solutions they can tailor to their specific workflows, rather than those that would require them to completely redesign how they operate. This means being able to modify fields, interfaces, and other elements as needed.
- HIPAA compliance: Data privacy should be top of mind for independent practices. As a result, Gaskins always ensures that potential vendors are willing to sign a business associate agreement (BAA).
Driving deeper human connections
Independent practices that follow Gaskins' mapping method and evaluation checklist adopt new administrative solutions quickly and effectively, allowing them to handle administrative work more efficiently while their larger competitors remain stuck in approval delays.
The impact is substantial: staff spend less time on routine tasks, which means they can see more patients per day while redirecting their mental energy toward higher-value clinical activities—comprehensive treatment plans, thorough assessments, and proactive progress management.
These improved outcomes translate into stronger patient retention and referrals, which drive sustainable revenue growth.
This shift in how clinicians spend their time creates a patient experience that's fundamentally different from what larger organizations can offer. Gaskins regularly hears patients describe how they feel like they're "running through the mill" at large health systems—but when independent practices have the bandwidth to build stronger, more personalized relationships, patients feel cared for as individuals rather than cogs in the healthcare machine.
These patients show better adherence to treatment plans, which improves outcomes while reducing the costly cycle of missed appointments and incomplete care episodes. They also stay with the practice longer and refer others, creating a sustainable growth engine.
The math is simple: better technology means more time for patient care, which means better outcomes and stronger margins. Independent practices that move quickly on the right solutions gain both a clinical and financial edge.