Tuesday, September 30, 2025
Don’t Choose Technology that Destroys Practice Productivity

Staff at independent rehab therapy practices are pulling their hair out over the administrative overload. While they’re calling on tech to help, many find that it actually makes the situation so much worse.
Christopher Gaskins, PhD, OTR/L, and CEO of mobile neurorehabilitation practice Neurosuite, has experienced the disruption and the discomfort it brings firsthand.
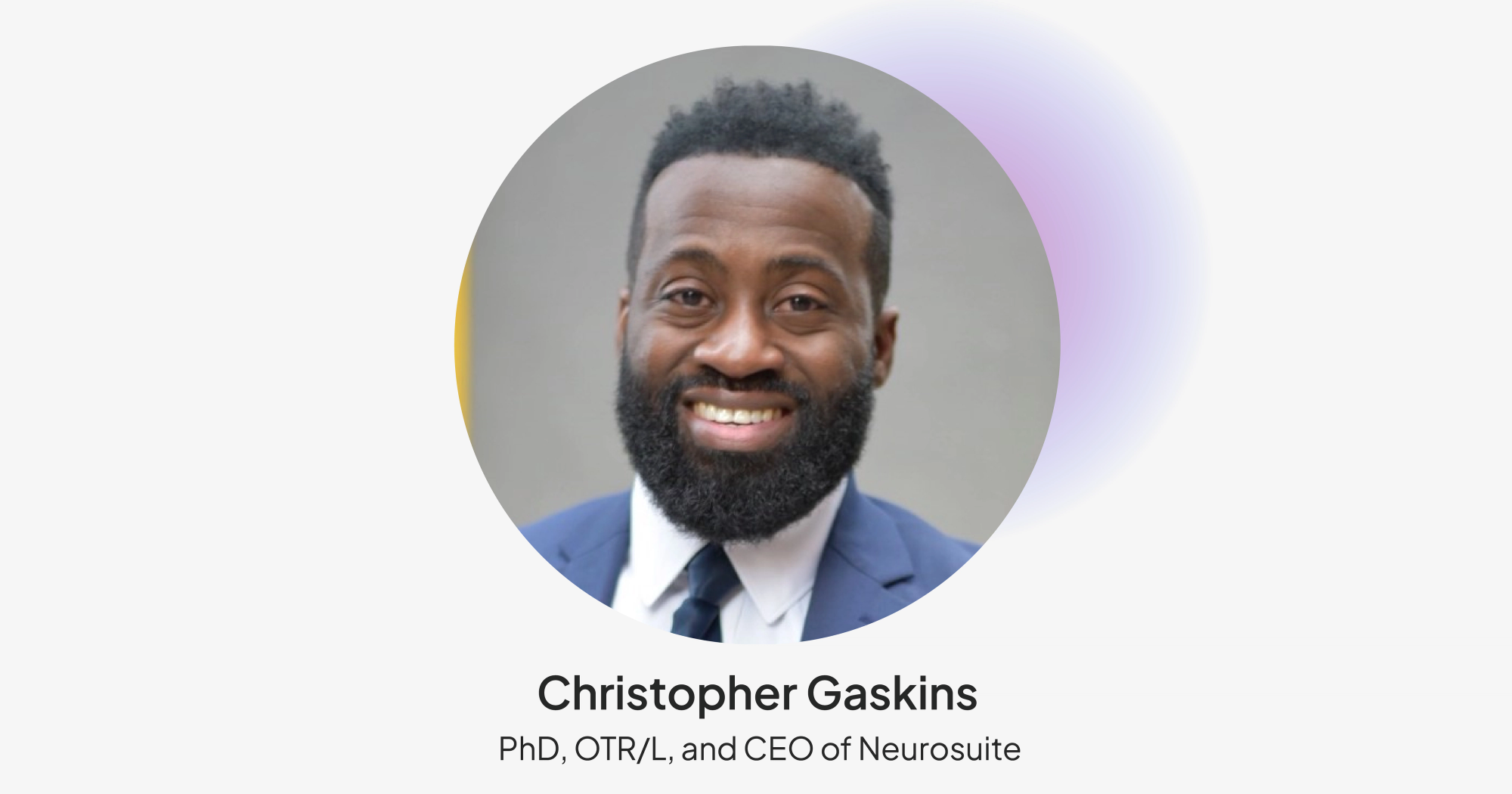
Drawing on his PhD research in cognitive load theory and years of hands-on clinical experience, Gaskins has learned how to prevent technology from creating additional problems for employees already overburdened with administrative tasks.
Key takeaways:
- When technology is implemented incorrectly, it increases the cognitive load on practice staff.
- Practices should ensure that new solutions fit into their unique operations to avoid putting more pressure on their hard-working staff.
- Achieving this alignment requires understanding existing processes before implementing or even selecting technology.
False promises
Many practices are struggling to keep up with documentation, pulling staff away from patient care while creating compliance risks.
Others are jumping through hoops to complete insurance verification. “I hate it. What we call insurance verification. Before we treat a client, we have to verify that they have insurance. We’re on the phone with the automated voice for 10–15 minutes. If you say one wrong word, one wrong letter, you have to do it all over again,” Gaskins explains.
Meanwhile, mobile practices, like Neurosuite, must navigate scheduling appointments across an expansive geographic area.
Some practices have the unfortunate responsibility of dealing with all of the above.
Technology promises relief, with tools like AI-powered scribes and automated scheduling platforms rising up to tackle the administrative burden. But Gaskins warns that these solutions can create more problems than they solve by disrupting workflows and introducing additional complexity that increases the cognitive load on already overwhelmed staff.
Whether tech helps or hinders often comes down to how it’s implemented. “Even with technological advances, technology is not being implemented correctly,” Gaskins observes. “This ends up placing more cognitive load on the user without the added benefit of improved performance.”
“Even with technological advances, technology is not being implemented correctly. This ends up placing more cognitive load on the user without the added benefit of improved performance.”
Time for some self-reflection
Technology should help streamline key tasks without placing additional pressure on the people who use it.
To avoid adding to the cognitive load, practices should ensure that new tools fit into their unique operations. When solutions align with existing workflows and technology, they blend into day-to-day tasks rather than disrupt them. This allows practices to benefit from increased efficiency without weighing on the mental bandwidth of their staff, truly freeing them to focus more on patient care and business growth.
According to Gaskins, achieving this alignment requires establishing a deep understanding of existing processes before implementing or even selecting technology.
How to adopt new technology without increasing cognitive load
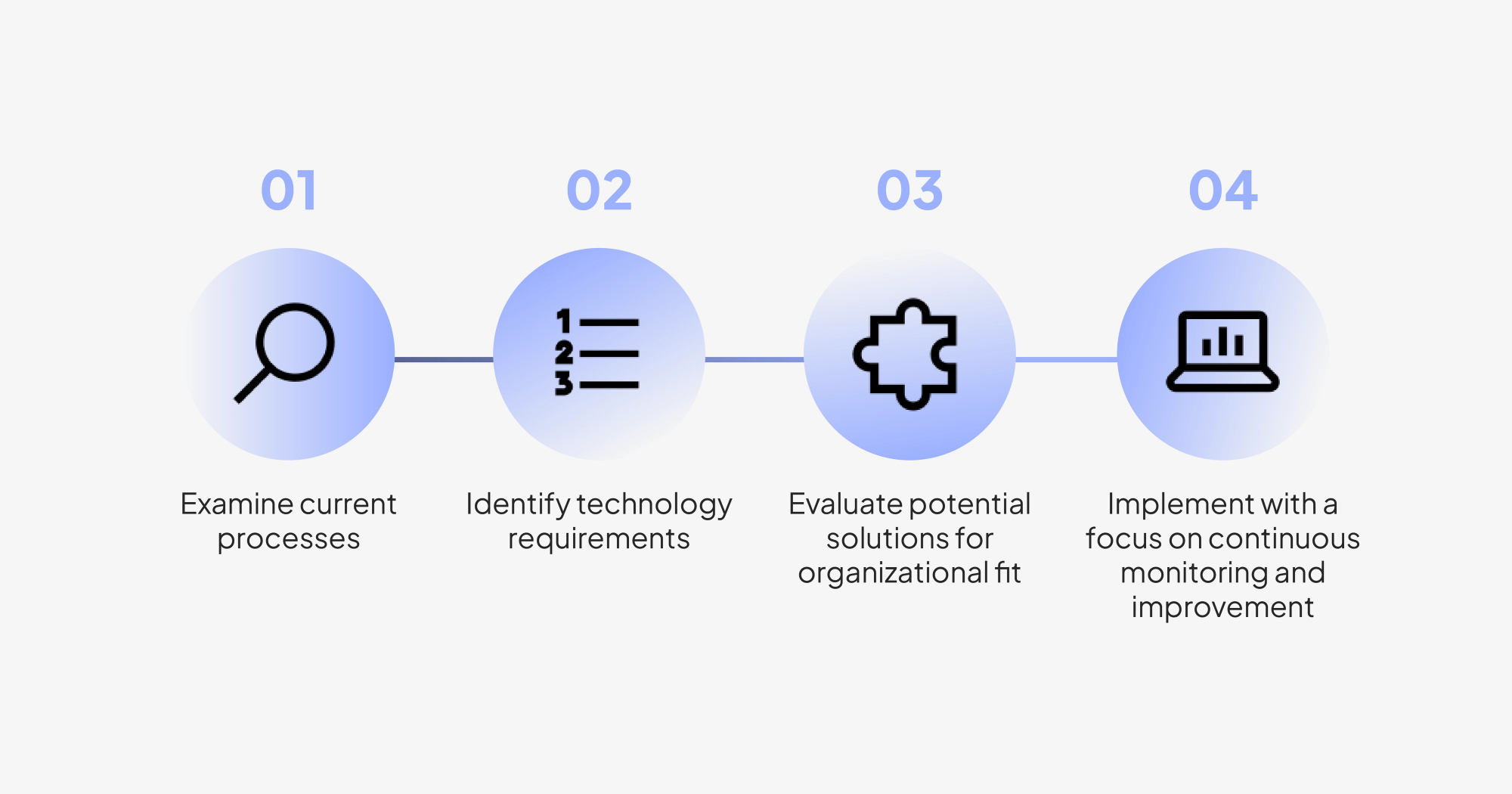
Step 1: Examine current processes
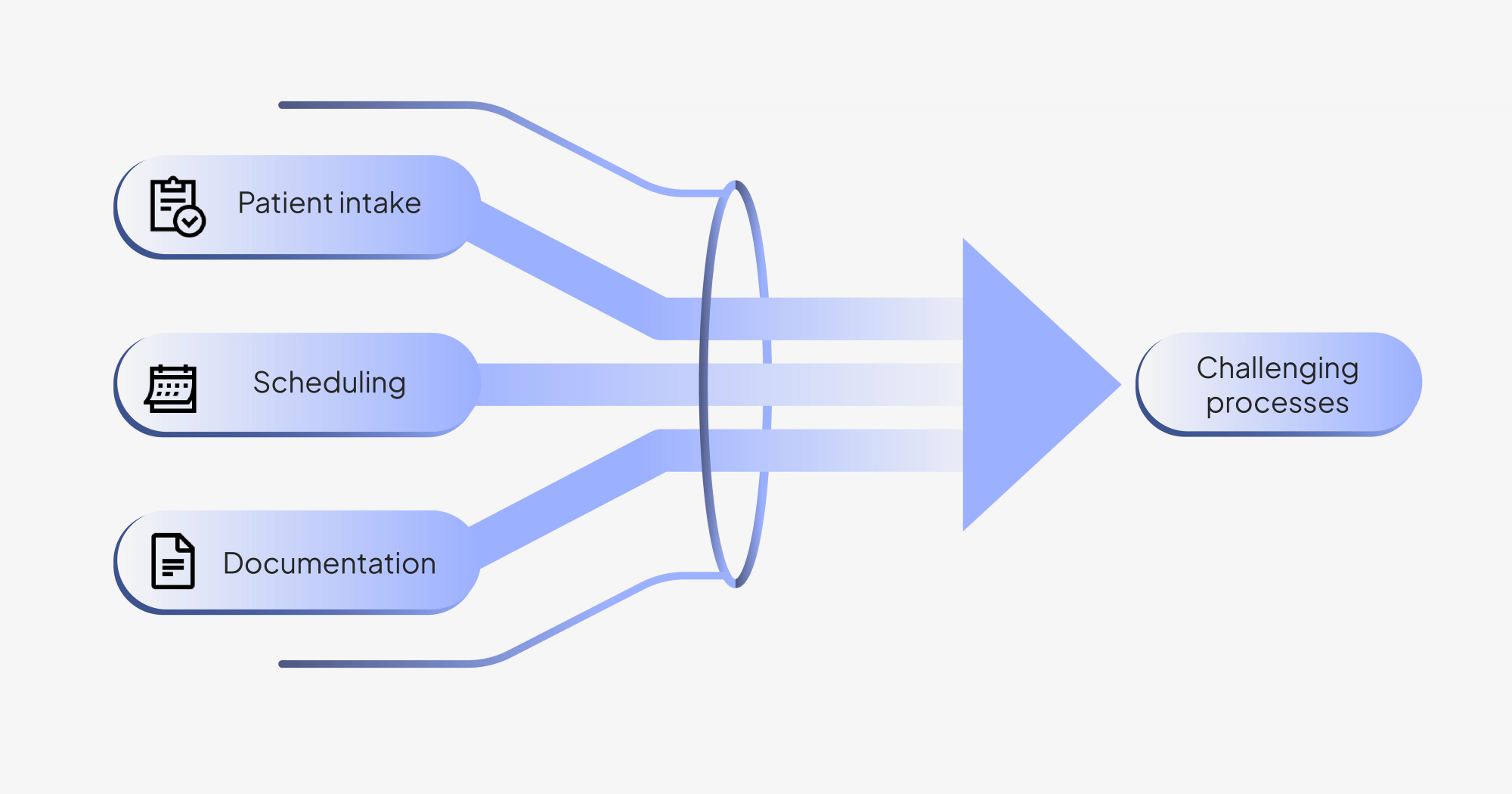
Practices should start by identifying processes that take the most time or generate the most errors. Patient intake, scheduling, and documentation often surface as being particularly challenging.
They should develop a clear understanding of how these workflows operate and where bottlenecks exist. One effective way to achieve this is through process mapping. Gaskins recommends creating diagrams that visualize how these workflows play out, step by step. This mapping exercise helps uncover the root cause of inefficient or error-prone workflows.
For practices that are unsure where to start or want an objective outside perspective, operational audit services can help assess workflows and bottlenecks. For example, Indie Health provides audits that typically include a complete mapping of front desk and billing processes.
Step 2: Identify technology requirements
Having established a deep understanding of their current processes, practices can determine where technology intervention will have the greatest impact. Knowing the exact problems they face helps better inform the types of solutions they need.
Before evaluating potential vendors, practices should also establish any non-negotiable requirements. HIPAA compliance is top of mind for Gaskins, so he always ensures that vendors are willing to sign business associate agreements (BAAs).
“A BAA is key. I think a lot of clinicians don’t care about it or don’t know that they need to care about it,” says Gaskins. “But that’s critical for me. If a vendor doesn’t have it, it’s a non-starter.”
Step 3: Evaluate potential solutions for organizational fit
Rather than getting caught up in the draw of advanced product features, practices should evaluate potential solutions against their documented processes and non-negotiable requirements. They need to ask themselves whether the tools they’re considering will actually solve the challenges they’re up against.
Practices should also prioritize tools that integrate with their existing platforms to avoid creating data silos and duplicative work. When evaluating potential solutions, Gaskins asks, “Is this system able to communicate with my other systems? Is everything interconnected?”
Beyond integration, Gaskins looks to see if solutions are customizable. This signals that solutions are flexible and can be adapted to align with unique organizational workflows, even as they change over time.
Step 4: Implement with a focus on continuous monitoring and improvement
When it comes to implementing new technologies, practices can’t just set them and forget them. They need to monitor performance to ensure that they’re working as intended.
Practices should establish clear success metrics to help measure efficiency gains, like time savings and error reduction. Meanwhile, practices should also routinely check in with staff to get a sense of how mentally taxing solutions feel during daily use.
Stress less, do more
When practices take the time to understand their processes before implementing technology, they can avoid creating additional complexity and free their people to focus on higher-value tasks.
When Gaskins evaluated his own workflows, he focused on scheduling, given that it was a major challenge for his mobile practice. Managing appointments across the sprawling DMV area, with patients in Washington DC, Maryland, and Northern Virginia, is no easy feat — and it was getting in the way of his ability to serve patients who desperately needed neurological rehabilitation.
He recognized that he needed a solution equipped to handle his unique circumstances. Rather than turning to a standard scheduling tool, he opted to run a custom AI analysis. The geographic clustering matrix he implemented dramatically reduced the time he spent scheduling appointments and traveling between them, without adding to his cognitive load.
And the results completely changed how he operates, letting him see more patients who need his specialized care without having to wrangle with all the location issues. No more logistical nightmare.
What his experience shows: Technology should amplify human capabilities. When practices investigate their unique challenges and select solutions that truly fit their operations, they’re not just cutting back on administrative burden — they’re making it possible to deliver better patient care.