Thursday, September 11, 2025
Independent Healthcare Practices Can Balance Purpose and Profit


There’s a destructive myth bouncing around the healthcare industry: Pursuing profitability inherently compromises patient care. Independent rehab therapy practices have absorbed this belief so deeply that even discussing profit can trigger suspicions of cutting corners.
“If you talk to some clinicians and use the word profit, they’ll assume you’re sacrificing quality of care,” says Eddie Czech, CEO and co-founder of Indie Health. Working with independent practices has also shown him that this assumption couldn’t be further from the truth.
He emphasizes that business health and patient health are heavily intertwined, with profit serving as an essential element of patient care.
Key Takeaways:
- Pursuing profitability and maintaining quality patient care are not inherently contradictory.
- Profit actually has the potential to drive better patient outcomes, especially when generated through operational efficiency improvements.
- Indie Health CEO Eddie Czech has developed a framework that shows practices how to treat efficiency as a gateway to profitability and better patient care.
You can’t help patients if you’re broke
The profitability myth carries real weight. Independent practices care deeply about their patients, so they internalize the message that focusing on profit is harmful.
As a result, Czech highlights that many overlook revenue-generating activities, leaving their finances highly susceptible to external market forces. Even in good times, this is suboptimal. But in challenging times, like right now, this is catastrophic.
While reimbursement rates fall, insurance policies are becoming more complex, sending administrative costs through the roof. The practices that haven’t prioritized profitability face unbearable pressure on their margins.
But the underlying belief that profit hurts patient care still remains unchanged, leading many practices to ignore the internal levers they can pull for relief, like adding cash pay options, upselling patients on additional services, or deploying new tech to improve operational efficiency.
This avoidance weakens their financial position, threatening business continuity and, in an ironic twist, their ability to care for patients.
Profitability is an essential element of patient care
Czech argues that practices must recognize that profitability and quality patient care are not mutually exclusive.
They actually reinforce one another, particularly through operational efficiency. “Finding efficiency in your business does not mean that the quality of care has to suffer,” Czech explains. “In fact, the quality of care will improve when you have more capital you can invest back into how you treat your patients.”
"Finding efficiency in your business does not mean that the quality of care has to suffer. In fact, the quality of care will improve when you have more capital you can invest back into how you treat your patients."

When practices generate profit by elevating operational efficiency, they aren’t cutting corners. They’re eliminating administrative waste and allowing staff to focus on patients while building the financial strength to invest in better care.
While this isn’t the only strategy available for profitable growth, it’s one of the most accessible. “Almost everyone has an opportunity to drive more efficiency in their practice,” Czech notes. “But to do that, you have to think about where you can automate and how you can make more informed decisions.”
Czech has developed a framework that shows practices how to treat efficiency as a gateway to profitability and better patient care.
The Efficiency-First Framework for Profitable Practice Management
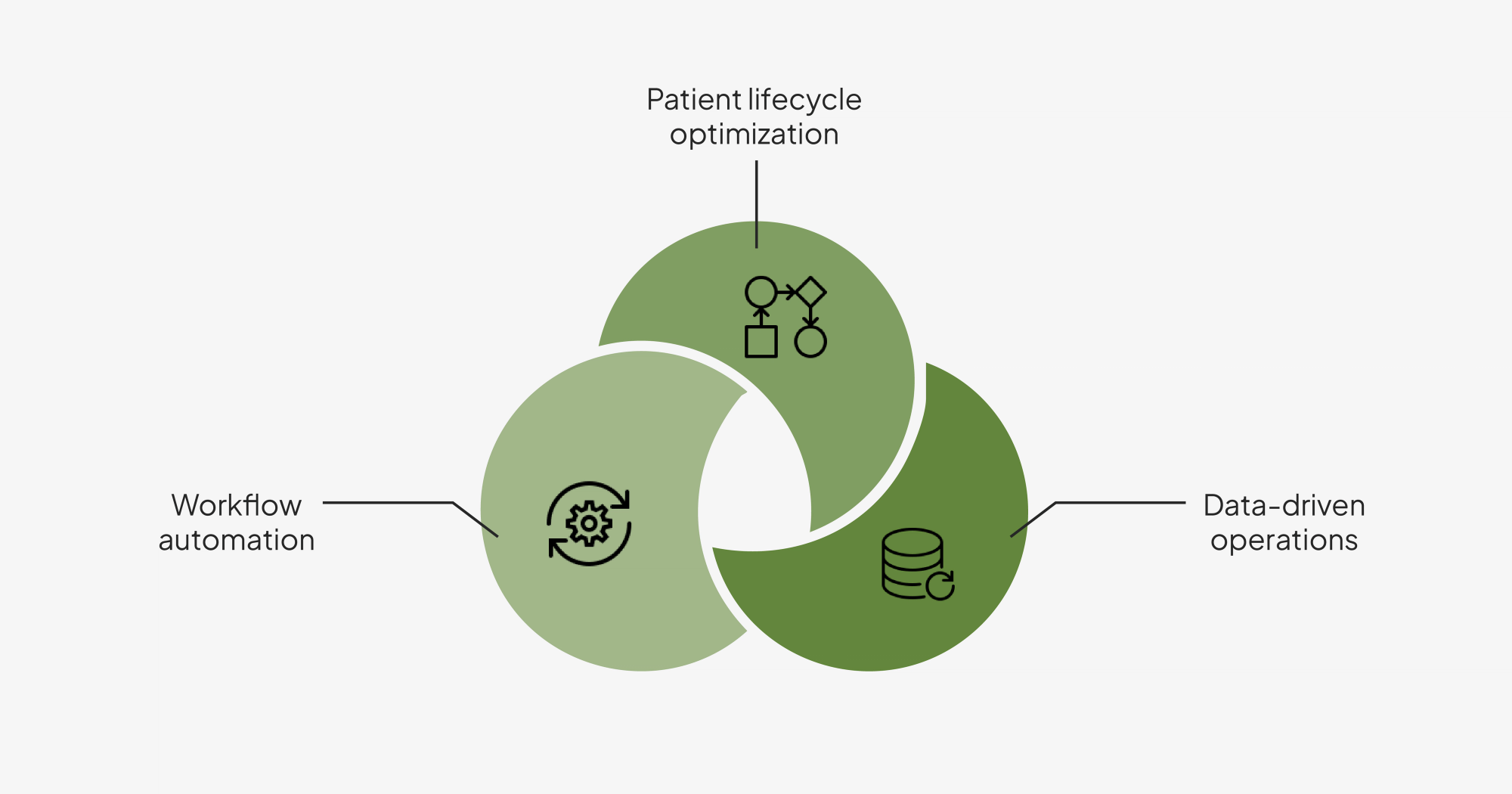
Workflow automation
Czech’s framework is rooted in eliminating administrative waste and freeing staff to focus on higher-value tasks. For Czech and the team at Indie Health, this means automating time-consuming, manual processes, like patient intake, billing and coding, and clinical documentation.
“Our system will record the sessions with the patients and generate notes, whether it's a SOAP note or an eval,” explains Czech. “And that dramatically cuts down documentation time for the clinicians, by 1–3 hours per day.”
This addresses a major problem providers face. Many fall months behind on documentation, leading to issues with claims processing and potential audits. One Indie Health customer had clinicians working through their holiday break solely to catch up on notes.
Automation can help practices recover this lost productivity, allowing staff to focus more of their time on patients (more on this in the next section) and ensure the timely submission of claims. When claims are continuously submitted on time, practices can prevent delays and denials, improve cash flow, and reinvest in patient care.
To take advantage of advanced automation tools, practices must implement a modern practice management foundation. Learn more in our tactical playbook.
Patient lifecycle optimization
When staff aren’t buried in administrative tasks, they can redirect their time toward patient engagement.
While patient acquisition is an essential activity, practices must also use reclaimed time to drive retention and maximize the value of their existing patient relationships. “Your current customer is worth way more than a new customer,” Czech warns. Yet, these patients tend to fall through the cracks.
"Your current customer is worth way more than a new customer.”

Patients typically only complete a portion of their treatment plan, dropping off after just a few of their approved sessions.
Czech recommends using telehealth, remote monitoring, and automated communications (SMS and email) to engage with patients between sessions and keep them connected to their care plan. These tools also help providers give their undivided attention to their patients, driving better treatment outcomes through delivery of exceptional care and, consequently, revenue growth for practices.
Data-driven operations
Most practices operate without visibility into key performance metrics. Typical blind spots include lead generation and conversion, appointment management, patient documentation compliance, treatment completion, and revenue forecasting.
“If I talk to 10 practice owners, maybe eight or nine don’t have visibility into some of that data,” he reveals. “This makes it really difficult to run a business.”
Without insight into these metrics, it’s impossible for practices to evaluate the effectiveness of their operational efforts. Practices must know what’s working (and what’s not) to ensure that they’re driving efficiency and that it’s translating into profitability and positive patient outcomes.
Czech emphasizes the importance of establishing data-driven operations with strong reporting infrastructure, like real-time dashboards. This allows practices to monitor acquisition, utilization, and cash flow patterns and act on them accordingly.
“Having insights is really important for identifying and fixing inefficiencies, spotting growth opportunities, and making smarter decisions about how to run the business,” he shares.
Staying in control of patient care
Czech’s efficiency-first approach demonstrates that the pursuit of profitability is far from being inherently harmful to patients. It’s advantageous.
By prioritizing operational efficiency, independent practices can generate revenue in a way that enables them to do more for the patients they serve now and down the road.
This approach provides them with time and money they can immediately reinvest in their patients. Beyond this, it grants practices true independence. As consolidation sweeps the industry, practices with thin margins are increasingly subject to ways of working imposed from the outside.
But the practices with strong financial standing can continue operating under their own values and goals, providing patient-centered care on their own terms during turbulent times.