Thursday, August 14, 2025
How to stay profitable as reimbursement rates plummet

Want your independent practice to stay profitable? Look beyond reimbursement rates
Reimbursement rates are falling, and there’s nothing independent rehab therapy practices can do about it. But that doesn’t mean profitability needs to suffer.
Informed by his experience building business management technology and navigating healthcare complexities, Indie Health co-founder and CEO Eddie Czech has developed an approach that can help these practices protect their margins. It requires looking beyond reimbursement rates, acknowledging other forces at play, and focusing on a factor they can actually control: operational excellence.
Key takeaways:
- Independent rehab therapy practice margins are becoming dangerously thin in the face of falling reimbursement rates, rising insurance complexity, and climbing operational costs.
- To survive and thrive in this environment, practices need to focus on what they can actually control: operational excellence.
- Operational excellence translates into the profitability practices require to retain control over their future.
No money, no options
Independent rehab therapy practices are in a tight squeeze that threatens their survival.
While reimbursement rates fall, complex insurance rules are creating administrative complexity and driving up operational costs.
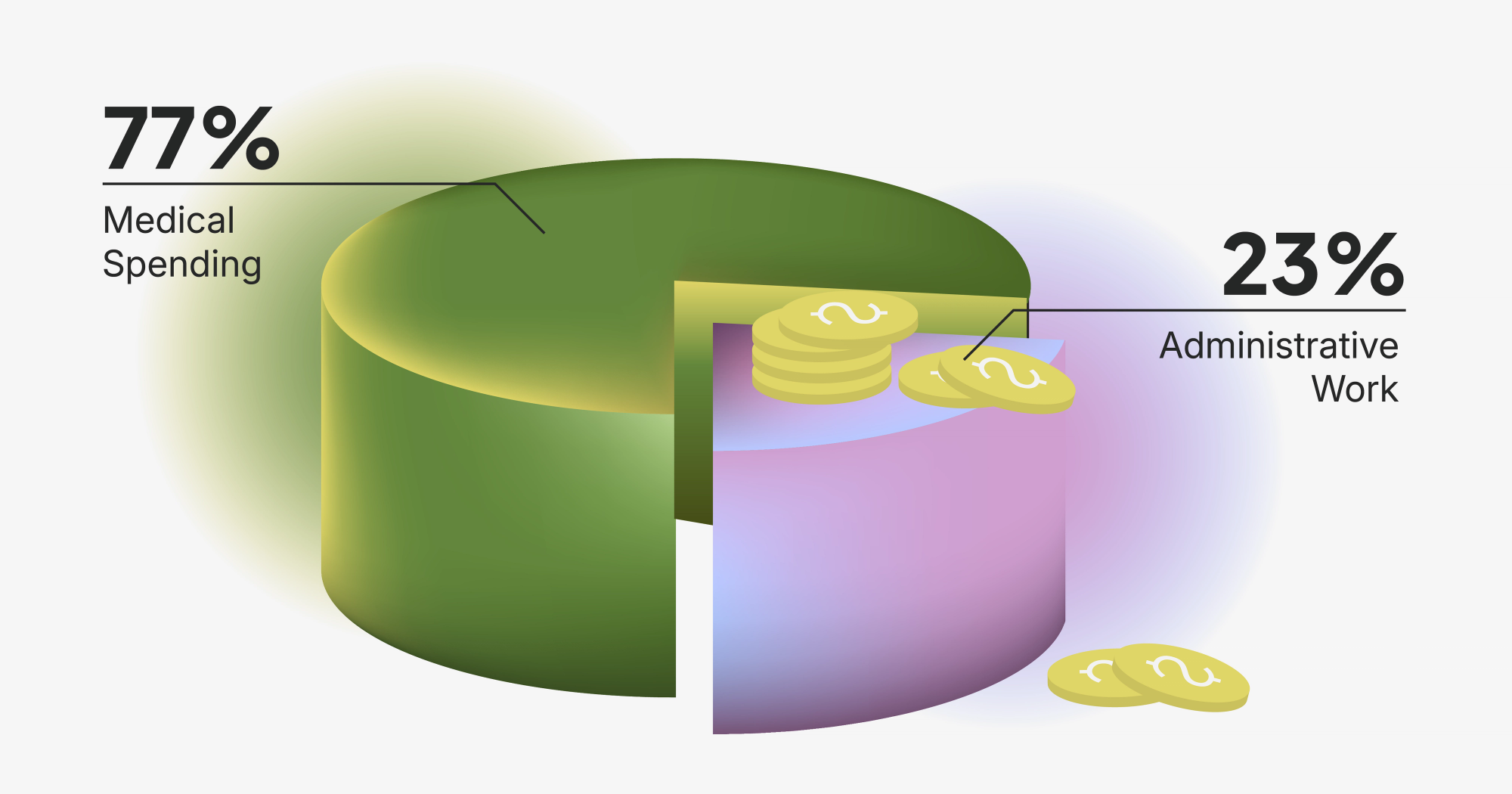
“For every dollar that's spent on healthcare in the US, about 23 cents goes to administrative work. And that number is going up,” says Czech. About a quarter of that administrative spend is “dead money,” i.e., costs that aren’t accounted for and don’t provide value.
While profits evaporate and costs swell, employee burnout intensifies, patient dissatisfaction climbs, and profitability suffers. Without the ability to reinvest in the practice, weighing options like operating on their own, establishing a health system affiliation, or pursuing a favorable sale is out of the question. Instead, practices are often simply left wondering how long they can stick it out before selling to private equity or another buyer.
In this scenario, they will largely be subject to the terms established by prospective acquirers.
This is when practices truly lose their independence, Czech highlights, when selling out of desperation becomes the only choice.
Look beyond falling reimbursement rates
To protect profitability and optionality in this environment, Czech encourages practices to focus on the factors they can actually control.
Setting reimbursement rates and insurance rules is out of their hands. However, practices can take the reins on operations to respond to those rules more effectively. By eliminating inefficiencies and optimizing key processes, practices will be better positioned to endure the uncertainty around them.
Czech underscores the importance of making this shift: “You're not going to survive unless you can find more efficiency in your business.”
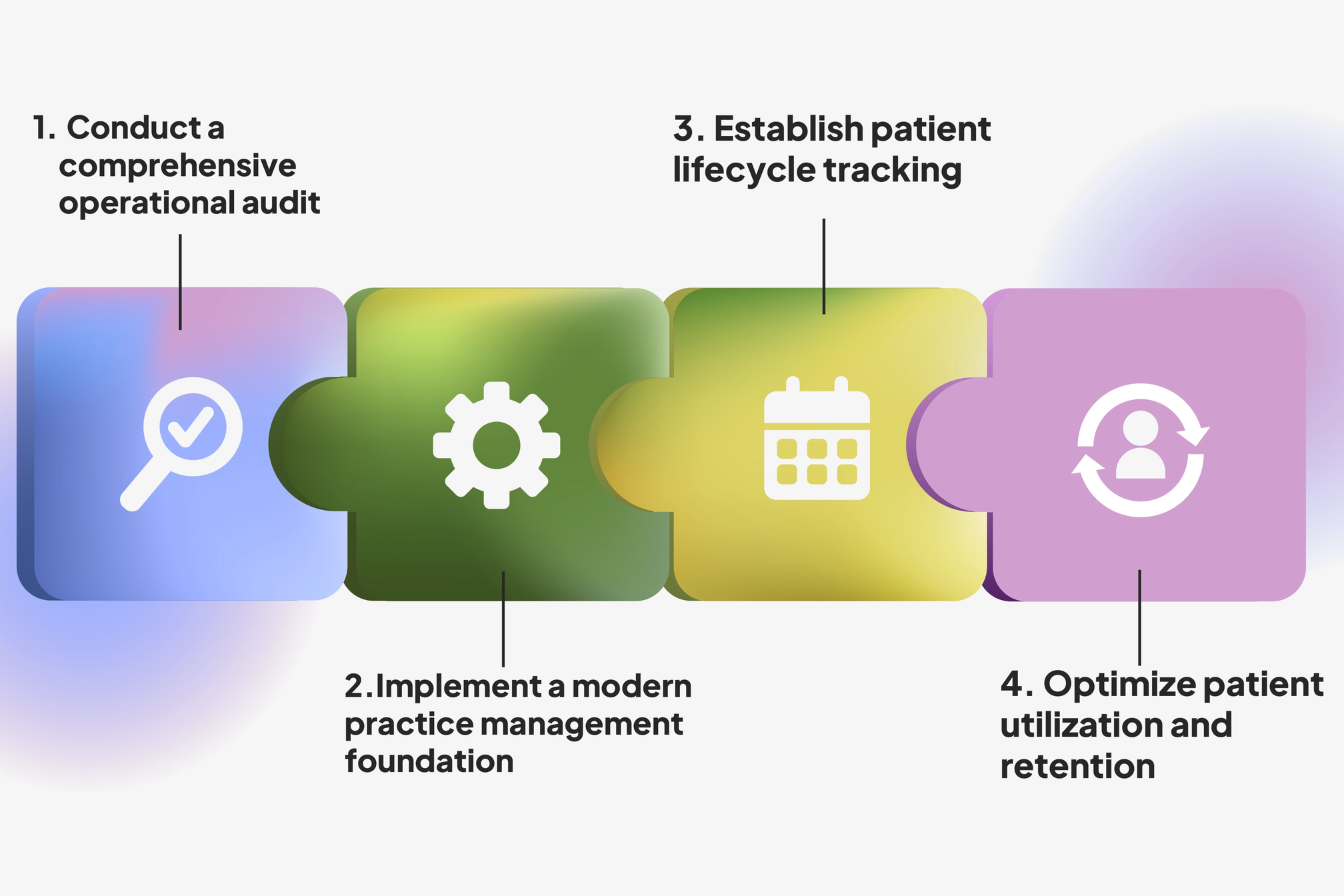
Here’s Czech’s four-step process for establishing operational excellence that drives sustainable profitability and genuine independence.
Achieving operational excellence: A survival guide

1. Conduct a comprehensive operational audit
Czech’s process starts with an honest assessment of current operations.
When working with practices, he prioritizes understanding existing operations before making any technology recommendations. From initial patient inquiry through final billing collection, this audit process requires documenting every workflow to identify resource-intensive manual processes that could be streamlined or automated.
Czech emphasizes that quick financial wins don’t always require new technologies. Simple operational adjustments, like evaluating staffing models for non-clinical roles, can have a significant financial impact.
“There are a lot of little things you could do to quickly optimize margins,” he states. “Handling these things first is non-negotiable.”
Once practices understand their current operations and have identified immediate efficiency gains, they can work on their technology foundation to drive a deeper transformation.
2. Implement a modern practice management foundation
Czech warns that many practices operate on outdated EMR and practice management systems. This makes it difficult to adopt new technologies that can help tackle resource-intensive processes. He highlights that legacy systems that merely “bolt on” AI features aren’t going to drive meaningful operational improvements.
Instead, practices need modern EMR and practice management platforms — those that support the integration of advanced tools for documentation, scheduling, billing, and claims management. Selecting a partner that can provide guidance at this stage is critical. “You need to partner with companies that are on the bleeding edge and understand which modern tools are required, how they work, and how they should be implemented,” says Czech.
Without modern systems and expert guidance, efforts to alleviate the administrative burden on employees and optimize the patient experience will fail.
3. Establish patient lifecycle tracking
Many practices lack visibility into critical business and patient information, inhibiting their decision-making.
Typical blind spots include:
- Lead generation and conversion: Number of phone calls from potential patients, what percentage convert to appointments, why leads don’t convert, and the most effective referral sources.
- Appointment management: Number of scheduled appointments and no-show rates.
- Treatment completion: The percentage of patients who complete their full, approved care plan and, for those who don’t, how many sessions they completed.
- Revenue forecasting: Expected revenue for the week, month, year.
Czech regularly encounters this gap when working with practices. “If I talk to 10 practice owners, maybe eight or nine don’t have visibility into some of that pipeline data,” he shares. “This makes it really difficult to run a business.”
Working with a technology partner, practices must implement CRMs that automatically track the complete patient journey, from initial contact through treatment completion, to drive more effective business decisions.
4. Optimize patient utilization and retention
Armed with patient data and free from the administrative burden of collecting it, practices can focus on maximizing the value of their existing patients. This prioritization is essential given that current patients are worth more than new ones.
Czech reveals that practices often uncover a utilization issue, with a typical patient only completing a fraction of their approved care plan. “If a patient gets approved for 10 sessions, they’re typically only going to go to three,” he illustrates. This represents a significant revenue leakage.
With the help of a technology partner, practices can effectively implement patient engagement solutions, like telehealth platforms, automated patient communication systems, and remote therapy monitoring, which, in some cases, may now be billable under updated codes.
These tools allow practices to stay connected with patients between sessions, encouraging plan completion and preventing drop-off. “You have to drive that number up, period,” Czech says, referencing the number of sessions completed. “Adding even just one or two sessions is beneficial. One of the best ways to do that is to think about all the things that you can do in between sessions to remind patients of the importance of their treatment.”
"Think about all of the things that you can do in between sessions to remind patients of the importance of their treatment."
Profitability will set you free
When practices achieve operational excellence using Czech’s four-step process, they can protect their profitability and uphold their independence.
Tackling inefficiencies and optimizing workflows can significantly reduce employee burnout by eliminating laborious, error-prone tasks. With 62% of doctors pointing to administrative work as their top source of burnout, per Medscape, these efforts can help practices appeal to top talent and retain their existing employees.
When administrative burdens are removed, clinicians and non-clinicians alike can focus more of their time on patient relationships, driving better compliance, outcomes, and referral generation. Independent practices already achieve 26% higher patient satisfaction than hospital systems, according to Czech, and operational excellence can help sharpen this edge.
Improvements in employee satisfaction and patient outcomes directly translate to enhanced financial performance in an environment where margins are under constant pressure. With greater profitability comes genuine practice independence — the power to choose how to move in the world.