Friday, July 25, 2025
25% of Your Budget Goes to Admin Work Your Staff Hates — Here’s How to Fix It
Indie Health co-founder and CTO Eric deRegt has spent years building technology solutions, including complex healthcare applications, and he’s noticed a troubling pattern: rehab therapy (OT, PT, ST, CT) practices struggling with administrative chaos that technology could easily fix.
Front-desk staff grapple with a series of manual tasks that require constant switching between several legacy systems.
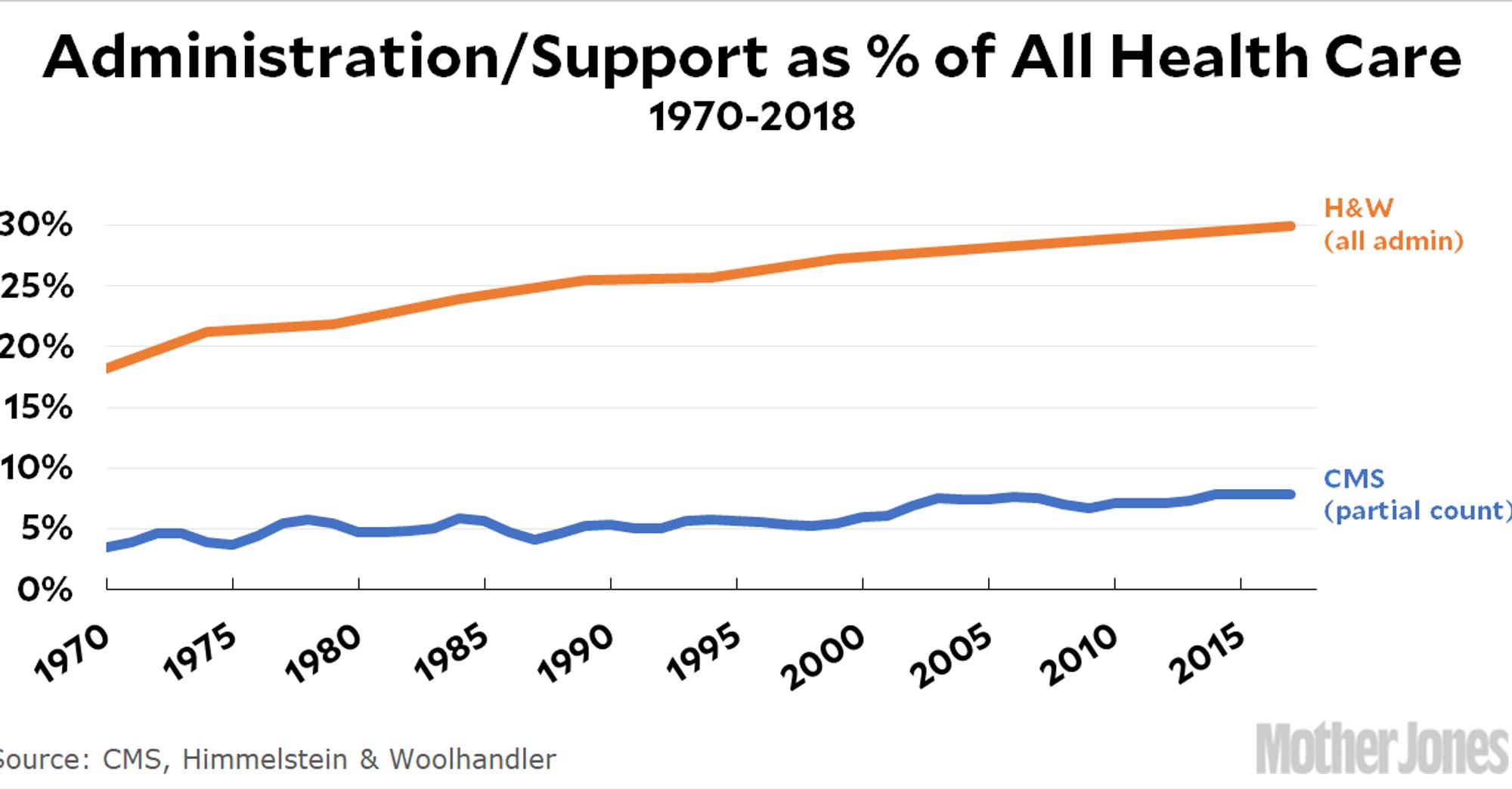
deRegt highlights that this administrative work can consume a quarter or more of practice spending. But it also creates operational inefficiencies that cause employees and patients to suffer.
As a result, practices are pumping resources into workflows that aren’t working for them, hurting their bottom lines.
By adopting healthcare-specific AI applications to automate and streamline key workflows, practices can shake the chaos holding them back. Free from the burden, they can regain their function and more effectively help their patients do the same.
But awareness of AI’s potential isn’t enough. deRegt has developed a practical framework to help practices navigate the vendor selection process. Keep reading to dive into his approach.
Key takeaways:
- Front-desk staff at rehab therapy practices are overwhelmed by manual tasks, creating operational inefficiencies that interfere with patient care and undermine profitability.
- By adopting healthcare-specific AI applications, practices can liberate the front desk, driving better outcomes for their employees, patients, and business.
- Eric deRegt shares a process-driven framework that practices can use to evaluate the capabilities of potential solutions.
Wasted time, wasted potential
Imagine a typical front desk at a rehab therapy office.
When an intake call comes in, the front-desk employee asks for all the information they’ll need to schedule an appointment, manually entering it into various systems or recording it on paper to upload later.
At the same time, the employee must navigate scheduling appointments, managing insurance verification, handling patient check-ins, and more — often on their own.
“It can be very chaotic at times,” deRegt says. “People are always calling in, and then you also have patients in the waiting room checking into appointments.”
The barrage of manual tasks invites error, like data entry mistakes or missed calls. It also doesn’t allow the employee to be fully present with the patient on the phone or those sitting in the waiting room. This prevents the employee from reaching their full potential — just think about the valuable tasks they could complete if they weren’t overloaded with administrative drudgery: building relationships with patients, implementing quality improvement initiatives, developing patient payment plans, and so much more.
The situation is not simply inconvenient for employees and patients; it also brings about downstream consequences, like:
- Employee burnout
- Patient dissatisfaction
- Issues with collections
- Lost business
These complications create a vicious cycle. They prevent practices from effectively carrying out their mission to deliver exceptional patient care while undermining profitability. With less revenue, practices are stretched thinner, making it even more difficult to deliver quality care.
Work smarter, not harder
Evaluating operational workflows at rehab therapy offices has shown deRegt that hiring more people, or forcing them to work harder, is not the answer.
Instead, practices should adopt healthcare-specific, ideally specialty-specific, AI applications to handle systematic, repetitive front-desk tasks. Whether these applications assist with or automate workflows, they can prevent errors with data capture and organization, improving data quality while freeing employees to be more present with patients.
deRegt emphasizes that the true promise of the tech lies in its ability to augment, not replace, employees. By tackling the grunt work, AI empowers people to take on higher-value tasks, allowing them to grow in their careers and drive growth for the practice.
However, AI implementation is often a black box. This leaves practices wondering what solutions they actually need, especially when so many options are available.
Demystifying front-desk AI implementation and its requirements
Drawing from his experience building complex healthcare applications, deRegt has developed a process-driven framework for evaluating them.
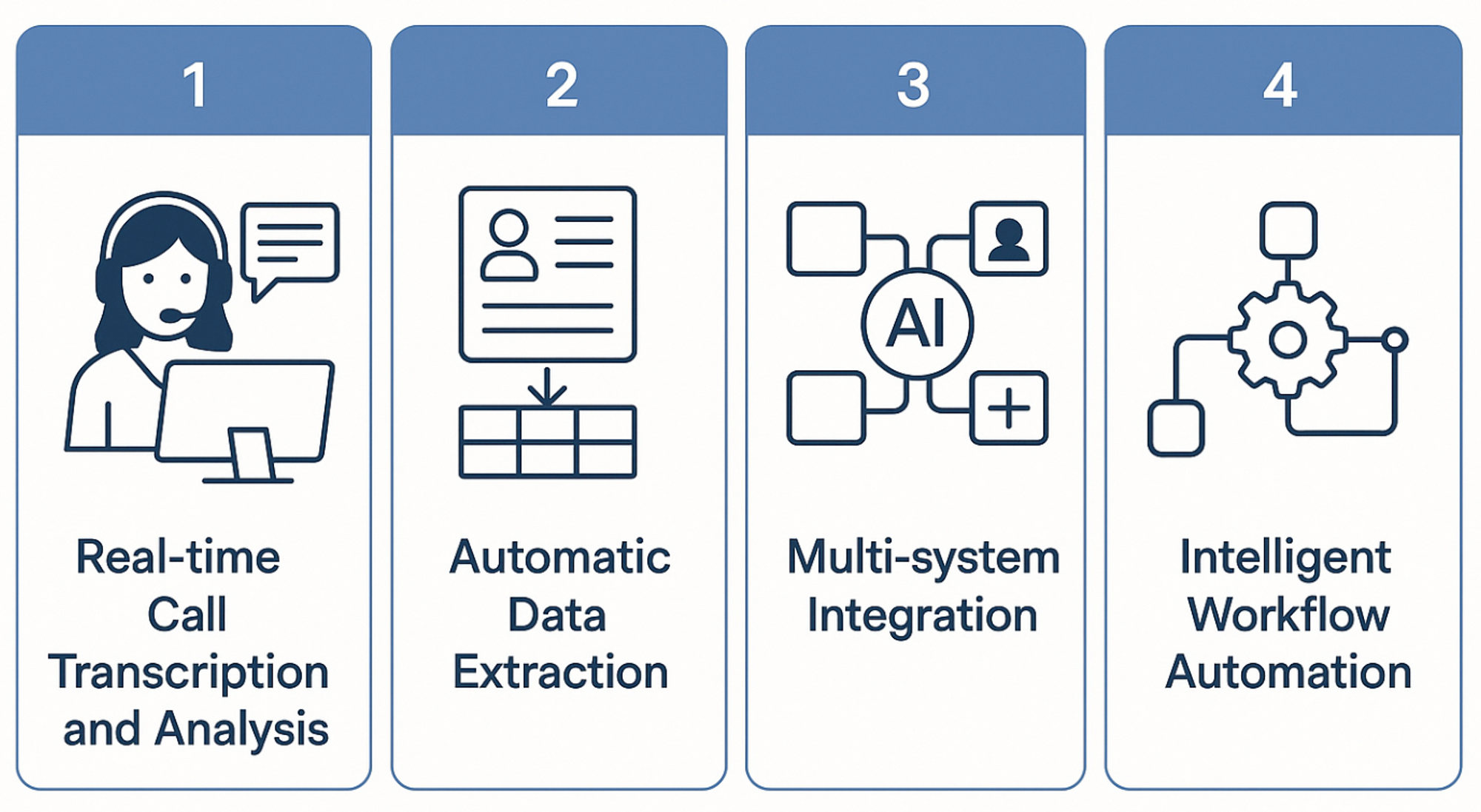
He breaks down front-desk AI implementation into four concrete stages to demystify the process and reveal the capabilities that practices should seek from potential vendors.
Stage 1: Real-time call transcription and analysis
The first stage of front-desk AI implementation is deploying real-time call transcription and analysis.
Practices should look for a solution that integrates with their existing phone systems to enable live transcription of calls. With this integration in place, employees can shift from frantically recording details to facilitating better conversations with patients.
In addition to transcription, deRegt highlights the importance of selecting solutions that can provide contextual support to employees while they’re on the phone.
Equipped with information on the business and the patient, these solutions can provide live suggestions to employees regarding:
- The information they should gather
- The questions to ask next
- How to ask those questions
Together, transcription and contextual guidance support more in-depth interactions, allowing practices to collect richer datasets while creating a more seamless experience for the patients they serve.
Stage 2: Automatic data extraction
Once data capture is covered, it’s time to address data entry.
Practices should look for AI applications that can be configured to automatically extract and organize patient information from calls to save time on input.
Working with practices, deRegt has witnessed how this capability can impact the post-call workflow, transforming downstream tasks, like appointment scheduling, into easy layups. “With Indie Health, you’ll automatically see all details from the interaction on your screen,” he shares. This includes patient information, like health history and insurance information, as well as potential appointment options.
This leaves employees with just one question to answer: Do you want to schedule this patient appointment? With one click, it’s done.
Stage 3: Multi-system integration
To drive effective data distribution, practices should look for AI applications that can connect to other practice management systems.
This includes but is not limited to:
- EMR platforms
- Scheduling software
- Billing systems
- Insurance verification tools
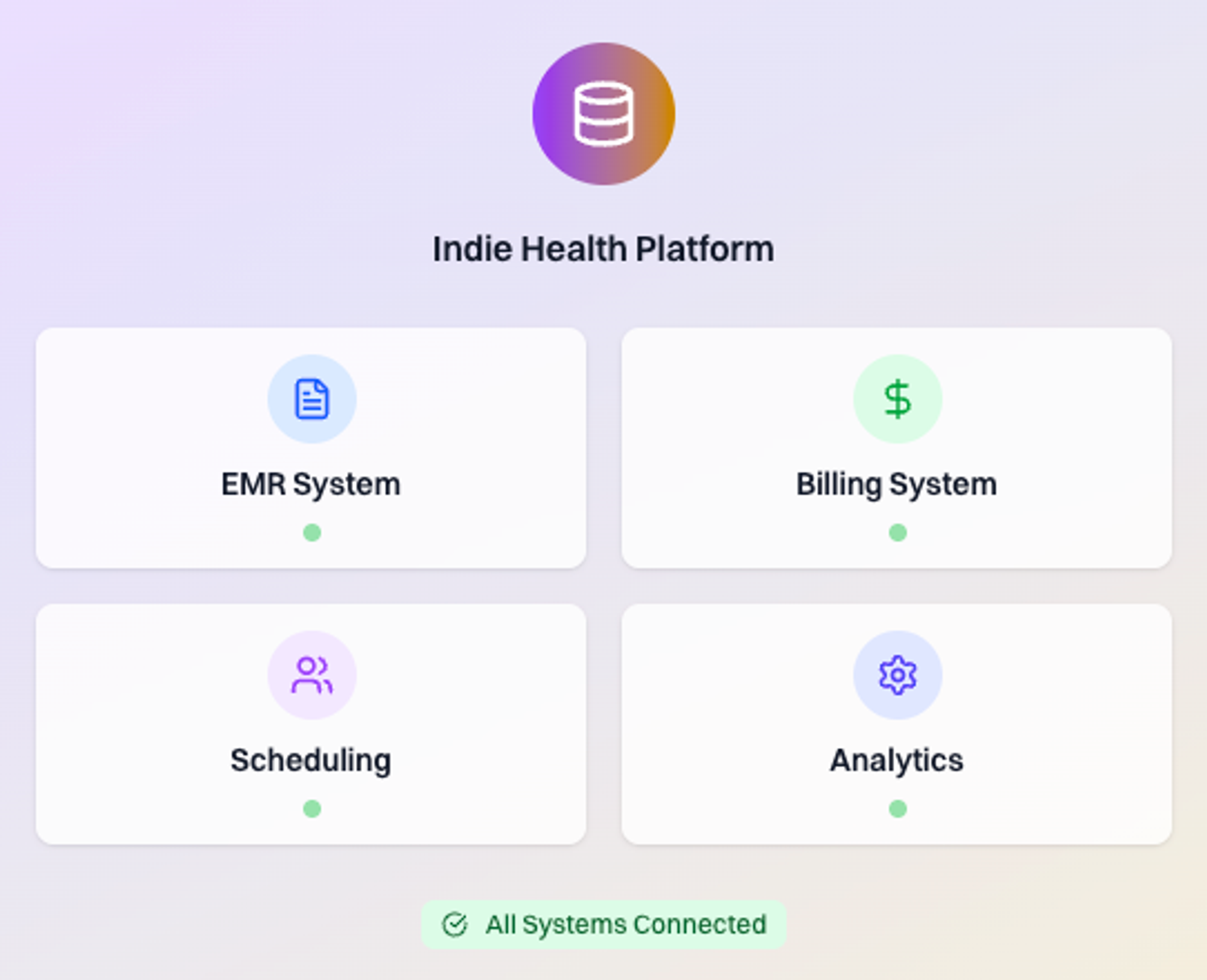
Establishing these integrations can be complex, especially when it comes to EMR platforms. But if they are set up properly, patient information will flow to where it’s needed and appear consistently in each location.
With robust data governance and a unified patient record, practices can get ahead of operational mishaps like missed appointments and billing errors. They can also prevent more serious incidents, like failed HIPAA compliance audits.
Stage 4: Intelligent workflow automation
The final stage of front-desk AI implementation is extending automation beyond data entry to encompass routine follow-up workflows.
Practices should focus on tools that can augment insurance verification, appointment confirmations, and other time-consuming tasks.
However, deRegt cautions practices to ensure prospective solutions leave space for human oversight, especially when streamlining tasks closely linked to regulatory compliance. In some cases, like obtaining prior authorization or modifying a treatment plan, he notes that solutions should enable AI-assisted workflows rather than full automation to ensure necessary provider reviews and approvals are completed.
Meant for more
By finding AI applications that can effectively support the four stages of implementation, rehab therapy practices can ease the administrative burden on their employees.
The transformation these applications drive is immediate and obvious. When showcasing Indie Health’s capabilities to practice owners and staff, deRegt notes that they are instantly blown away.
The thought of delegating time-consuming tasks is a big part of the draw.
However, he adds that this is equally matched by the promise that they can do so much more — for themselves, the business, and the patients they serve. “They have a list of other things they would rather be doing,” he observes. “These are tasks that could help them grow in their career and add value to the business.”